At Dr. Sudhir’s Pain Relief Clinic, we have always emphasized that stress is more than just an emotional state. It is a powerful biological force that can influence nearly every system of the human body. A new international study conducted by researchers at the University of Cambridge in the United Kingdom and the U.S. National Institute of Mental Health, recently published in Nature Communications (September 2025), adds a fascinating new layer to our understanding of stress. Their findings reveal that chronic stress can actually inflame the brain by activating the immune system in ways we never expected.
The New Discovery: Stress and the Immune System
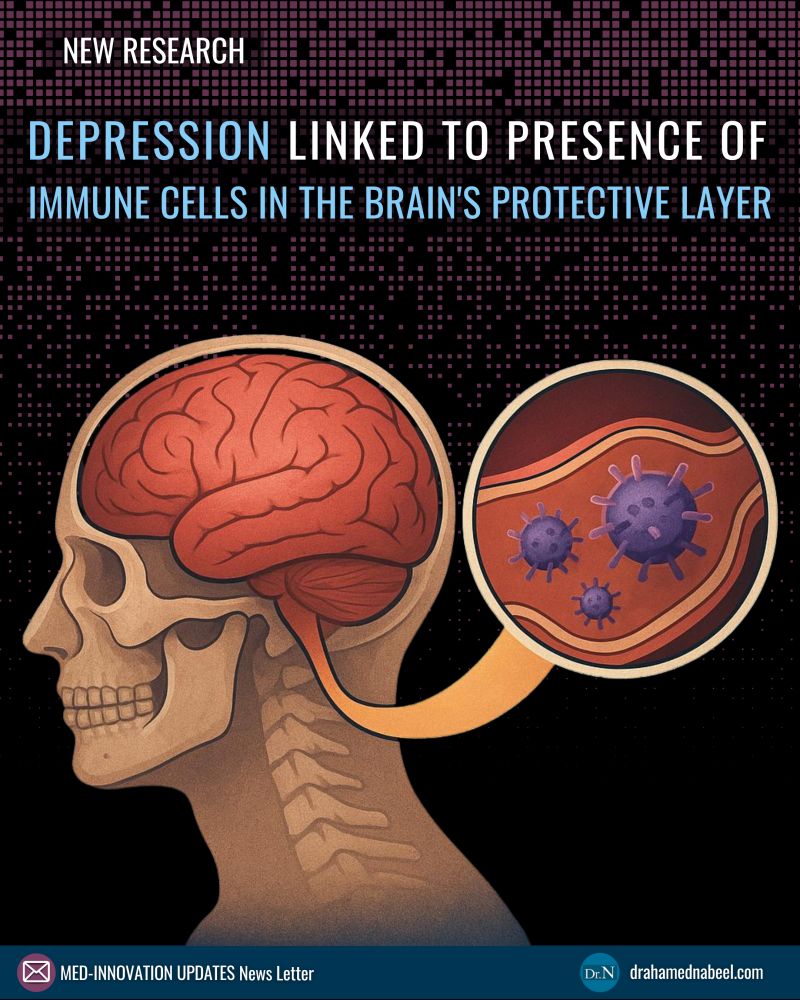
For decades, scientists believed that stress mainly acted on hormones and neurotransmitters in the brain. While that remains true, this study shows that stress can also trigger a direct immune response. Researchers discovered that chronic stress activates bone marrow inside the skull. This activation then produces neutrophils, which are a type of immune cell. Instead of remaining in the bloodstream where they typically function, these neutrophils travel into the meninges — the protective layers surrounding the brain.
Once there, these immune cells behave differently than usual. They remain longer than expected, become unusually active, and cause a form of prolonged inflammation. This immune activity was closely linked to behavioral changes in the experimental models, including symptoms that resembled depression.
Understanding the Process in Simple Terms
The chain of events can be summarized as follows:
-
Stress stimulates the bone marrow inside the skull.
-
This produces neutrophils, which then move toward the brain’s protective lining.
-
These immune cells accumulate and remain active in the meninges.
-
The prolonged immune response leads to inflammation, which in turn is associated with depressive-like symptoms.
This means that stress does not simply affect mood or thoughts. It has a direct, measurable impact on the immune environment around the brain.
Key Experiments That Shaped the Findings
To test whether this immune pathway could be modified, researchers blocked a particular signaling mechanism in the immune system, known as type I interferon signaling. When this pathway was inhibited, fewer neutrophils accumulated in the meninges. Most importantly, the associated depressive-like behaviors were reduced.
This result is highly significant because it demonstrates that the symptoms were not just coincidental but were directly connected to immune overactivation. By targeting immune–brain communication, the researchers were able to alter behavior and reduce the harmful effects of stress.
Why This Research Matters for Patients
The implications of this discovery go far beyond laboratory studies. Currently, around 30 percent of patients with depression do not respond well to conventional treatments such as antidepressant medications or psychotherapy. This condition is known as treatment-resistant depression, and it represents one of the biggest challenges in modern psychiatry.
The new findings open the door to an entirely different approach: focusing on how the immune system interacts with the brain. If future therapies can reduce immune overactivity in the meninges, it may be possible to offer relief to patients who have not found success with existing treatments. This could be the beginning of next-generation therapies that address not only brain chemistry but also the immune response that influences mood and behavior.
Clinical Perspective and Future Directions
It is important to note that this study was conducted in mice, meaning it is still pre-clinical research. Human studies are needed before we can fully understand how this process works in people and how safe or effective such immune-targeting treatments might be. Nevertheless, the research is highly promising and adds to the growing recognition that stress, inflammation, and mental health are closely linked.
At Dr. Sudhir’s Pain Relief Clinic, we are particularly interested in this connection because many of our patients experience both chronic pain and high levels of stress. Pain and stress often reinforce each other, creating a cycle that is difficult to break. This new research reinforces the importance of holistic care, where both the physical and emotional aspects of health are addressed together.
How We Approach Stress and Pain in Our Clinic
Our treatment philosophy goes beyond simply managing pain symptoms. We work with patients to address underlying stress, emotional wellbeing, and immune health. This may include advanced pain therapies, lifestyle guidance, relaxation techniques, and stress management strategies. By reducing stress and its biological impact on the body, we aim to help patients achieve not only pain relief but also a stronger sense of overall wellbeing.
Final Thoughts
The discovery that stress can activate bone marrow, recruit immune cells to the brain, and contribute to depressive symptoms is a striking reminder of how interconnected the body and mind truly are. The line between mental and physical health is not as clear as once believed. Instead, both exist in constant dialogue through the immune and nervous systems.
As science continues to uncover these connections, clinics like ours are committed to integrating these insights into patient care. Stress may be invisible, but its effects are very real — and with the right approach, both body and mind can be guided toward healing.
Call our specialists at +91 91636 95790.