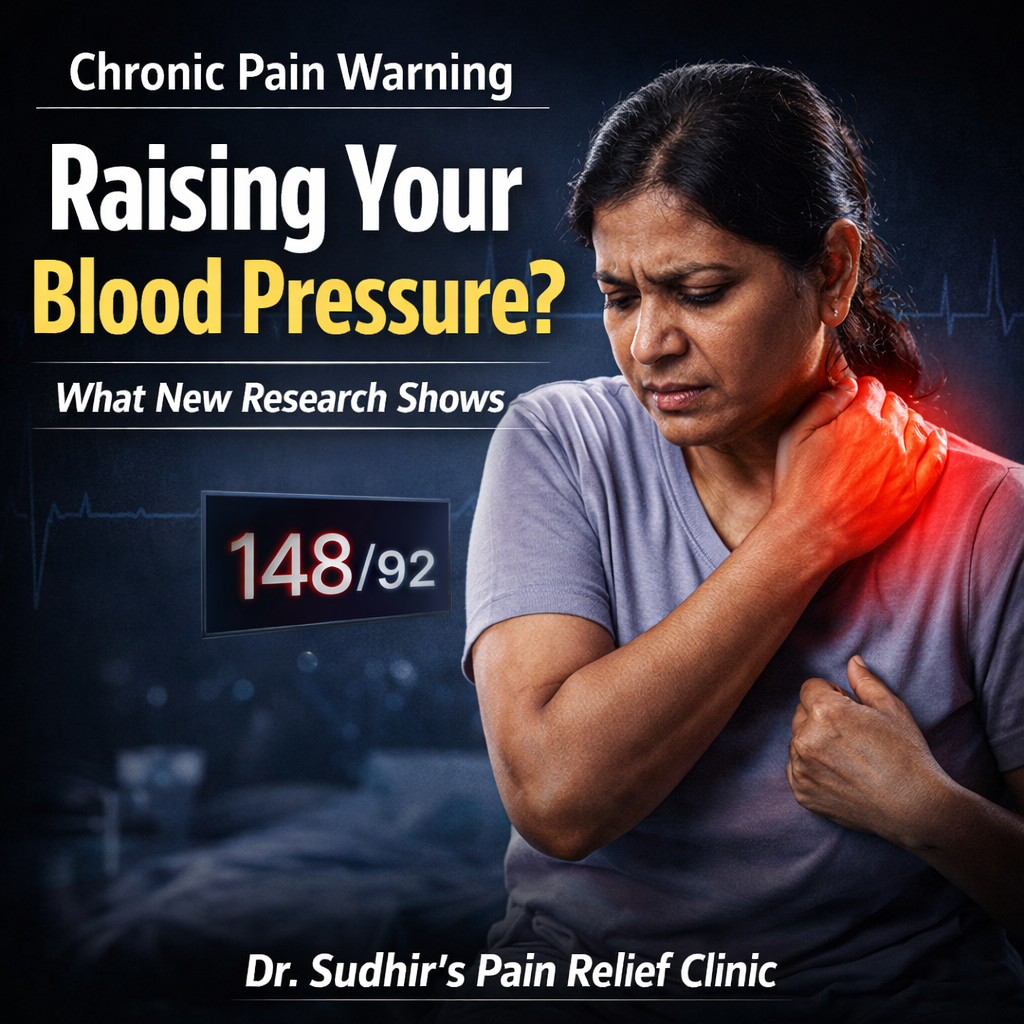
A new study is drawing attention to an important but often overlooked connection: people living with chronic pain may have a higher risk of developing high blood pressure (hypertension).
For many patients, pain is treated as a local problem — in the back, knee, neck, or joints. But growing research shows that long-term pain can affect the entire body, including the cardiovascular system.
Understanding this link can help patients take earlier action to protect their overall health.
What the New Research Suggests
Recent findings indicate that individuals with persistent or chronic pain are more likely to develop elevated blood pressure over time compared with those without ongoing pain.
Researchers believe the relationship is not accidental. Instead, chronic pain may trigger physiological changes that place continuous stress on the body’s regulatory systems.
The key message:
Chronic pain is not just uncomfortable — it may also increase cardiovascular risk.
Why Chronic Pain Can Raise Blood Pressure
Several biological mechanisms may explain this connection.
1. Constant Stress Response
When the body experiences ongoing pain, it activates the sympathetic nervous system — the same system responsible for the “fight-or-flight” response.
This can lead to:
increased heart rate
tightened blood vessels
sustained elevation in blood pressure
Over time, this persistent activation may contribute to hypertension.
2. Elevated Stress Hormones
Chronic pain often keeps levels of stress hormones such as cortisol and adrenaline higher than normal.
Long-term elevation of these hormones can:
stiffen blood vessels
increase vascular resistance
strain the heart
All of these factors can push blood pressure upward.
3. Poor Sleep in Pain Patients
Many people with chronic pain struggle with:
difficulty falling asleep
frequent nighttime awakening
non-restorative sleep
Poor sleep is a well-known contributor to high blood pressure and cardiovascular strain.
4. Reduced Physical Activity
Pain often causes people to move less. Lower activity levels can lead to:
weight gain
reduced cardiovascular fitness
poorer blood circulation
These changes further increase the risk of hypertension.
5. Chronic Inflammation
Long-standing pain conditions are often associated with low-grade systemic inflammation, which can:
damage blood vessel lining
reduce vessel flexibility
contribute to rising blood pressure
Who May Be at Higher Risk
Patients should be especially cautious if they have:
chronic back pain
long-term knee osteoarthritis
persistent neck or shoulder pain
fibromyalgia
nerve pain conditions
pain lasting more than 3 months
The longer pain persists, the more important whole-body monitoring becomes.
Warning Signs to Watch
If you live with chronic pain, pay attention to:
frequent headaches
dizziness
unexplained fatigue
sleep disturbances
rising blood pressure readings
feeling unusually stressed or tense
These may signal that pain is affecting more than just muscles or joints.
Why Managing Pain Early Matters
Proper pain management does more than improve comfort. It may also help:
reduce chronic stress load
improve sleep quality
support healthier blood pressure
restore normal nervous system balance
improve overall quality of life
This is why modern pain care focuses on whole-body recovery, not just symptom suppression.
What Patients Can Do Right Now
✓ Monitor Blood Pressure Regularly
If you have chronic pain, periodic BP checks are wise.
✓ Improve Sleep Quality
Aim for 7–8 hours of consistent, restorative sleep.
✓ Stay Gently Active
Even light guided movement can help circulation and nervous system balance.
✓ Manage Stress Levels
Breathing exercises, relaxation techniques, and proper pain care all help.
✓ Seek Professional Pain Evaluation
If pain is persistent, recurring, or worsening, early intervention is important.
When to Consult a Specialist
Consider professional evaluation if:
pain lasts longer than 12 weeks
pain is affecting sleep or daily activity
blood pressure readings are rising
you feel constantly tense or fatigued
pain keeps returning despite rest
Early, targeted therapy can help break the pain–stress–blood pressure cycle.
Final Thought
The new research reinforces an important truth:
Chronic pain is not just a local problem — it is a whole-body stressor.
Ignoring persistent pain may allow silent strain to build in the background. Addressing pain properly and early is not only about comfort — it is also about protecting long-term health.
If your pain has become a daily companion, it may be time to look beyond temporary relief and move toward a structured, professional recovery plan.